Fee For Service Reimbursement Systems Help Reduce Health Care Expenditures It is a consensus that Fee for Service FFS is a traditional medical insurance payment scheme with significant disadvantages namely the waste of health care resources
Reimbursement mechanisms for healthcare have included salary Fee for service FFS capitation Pay for performance P4P and diagnosis based payment DRGs diagnosis Comparing policies in three high income countries France Germany and Japan we describe how payers and physicians engage in structured fee negotiations and standardize prices in
Fee For Service Reimbursement Systems Help Reduce Health Care Expenditures
Fee For Service Reimbursement Systems Help Reduce Health Care Expenditures
https://www.ruralhealthinfo.org/assets/5014-22505/payment-and-reimbursement-fb.jpg

FACT SHEET Medicaid Is A Lifeline For People With Disabilities
https://www.protectourcare.org/wp-content/uploads/2024/03/Web-Metadata-v0.1-01.png
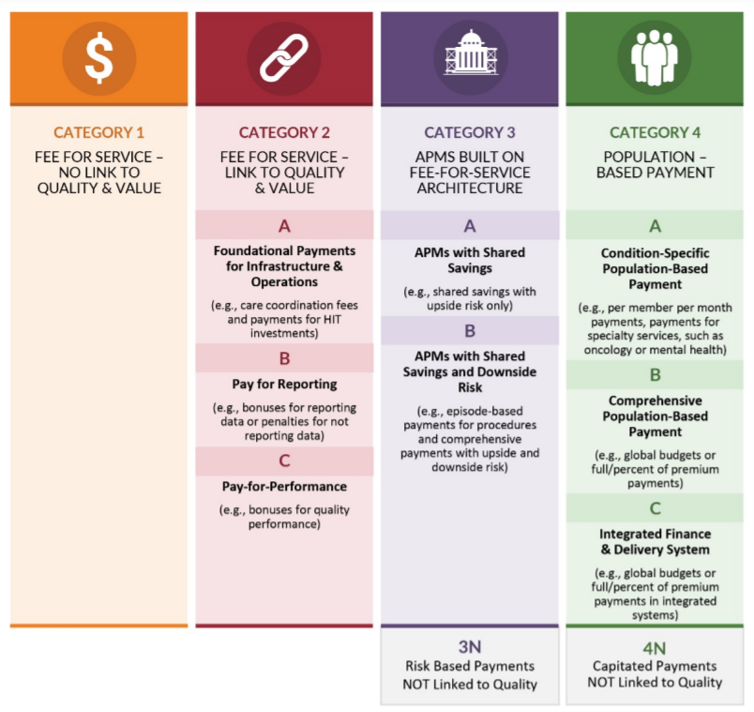
Alternative Payment Models Where Are We Now Healthcare Economist
https://www.healthcare-economist.com/wp-content/uploads/2021/12/APM-types.png
Comparing policies in three high income countries France Germany and Japan we describe how payers and physicians engage in structured fee negotiations and standardize prices in As reimbursement cuts lead to reductions in hospital revenues hospitals may decrease operating expenses reduce unprofitable care and increase profitable care to preserve profit 1 7 Strategies to reduce operating
In short fee for service is a traditional payment model where healthcare providers are reimbursed for each service they deliver to a patient while value based care is a newer approach that incentivizes providers to The transition from a fee for service FFS reimbursement system to one based on value is one of the greatest financial challenges for health systems Although there are too many transition
More picture related to Fee For Service Reimbursement Systems Help Reduce Health Care Expenditures
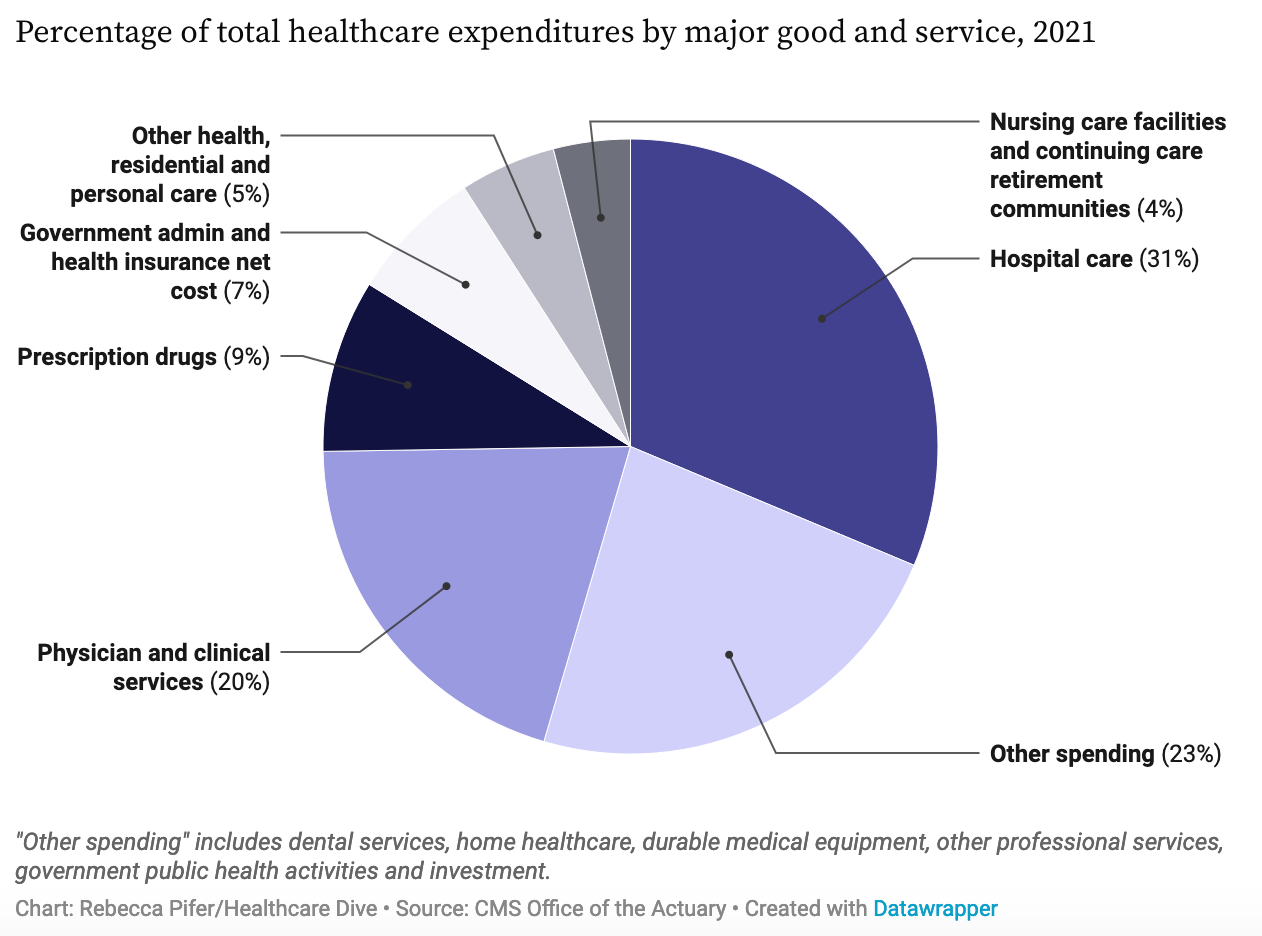
2021 US National Health Expenditures Healthcare Economist
https://www.healthcare-economist.com/wp-content/uploads/2022/12/Screen-Shot-2022-12-26-at-11.26.55-AM.png

Board Appoints New Executive Director Annie Knight Northern Waters
https://northernwaterslandtrust.org/wp-content/uploads/2023/07/Annie-Knight_Headshot-scaled.jpg

EXHIBIT 1 The Alternative Payment Model Framework
https://www.healthaffairs.org/do/10.1377/hpb20221014.526546/full/health-affairs-brief-value-based-payment_fig1-1669048653814.png
Fee for service rewards physicians with more revenue for rendering more services whether these services improve the health or well being of the patient Under FFS reimbursement services The current health care reimbursement system in the U S reflects challenges with the FFS model in light of rising industry costs the shift to value based care and the new reimbursement
Reforming our health care payment systems will have a dramatic impact on how health care is delivered and hospital based care in particular In this chapter we 1 address In a strategic plan refresh published in November 2022 CMS set a target of aligning 100 of Medicare fee for service beneficiaries with an accountable care relationship by 2030 Thus

Racial Health Disparities In Michigan Declined According To COVID Task
https://wdet.org/wp-content/uploads/2023/02/MicrosoftTeams-image-50-scaled-e1677602148241-2048x1152.jpg
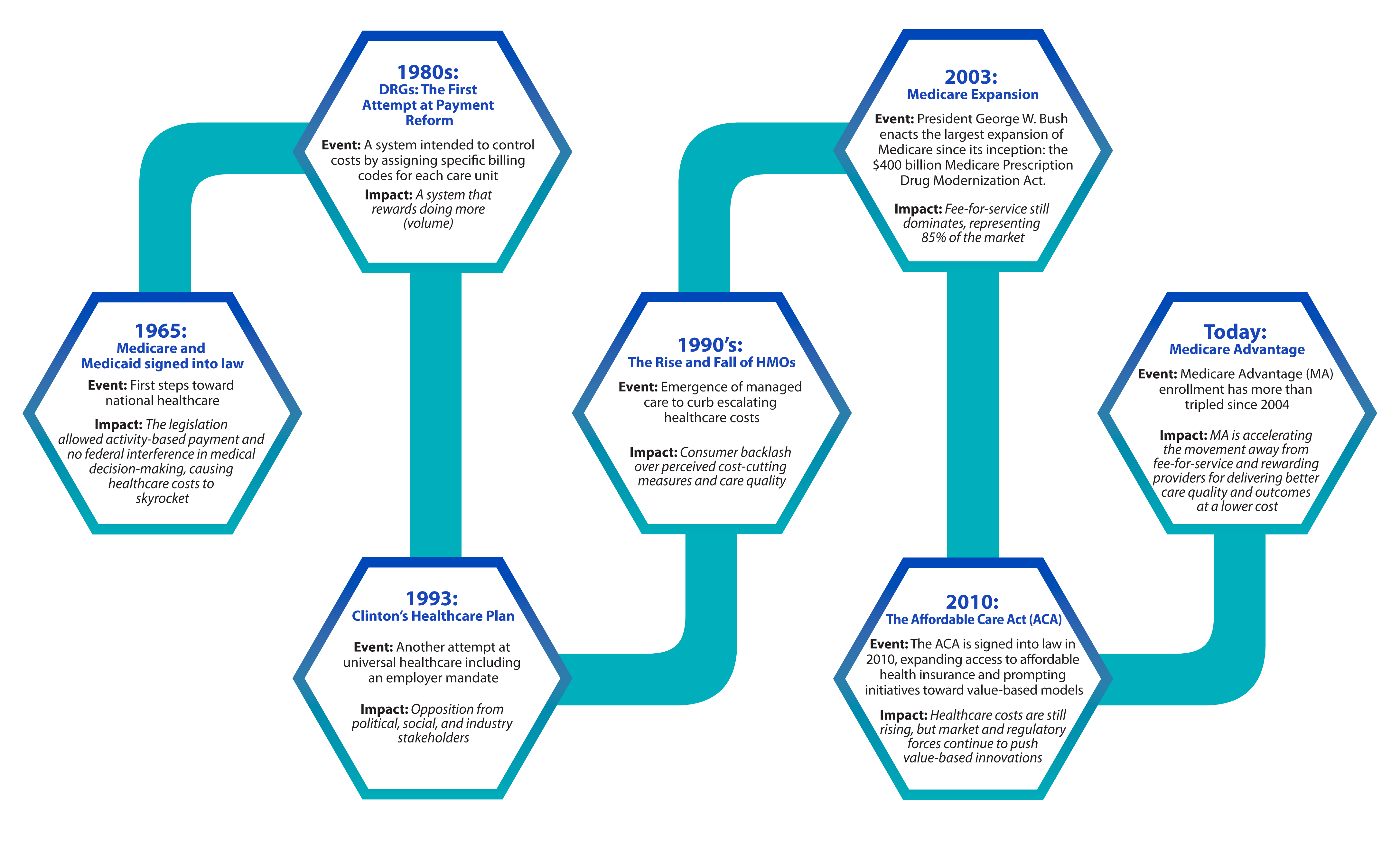
White Paper 40 Years In The Payment Reform Wilderness DRGs To Nirvana
http://www.lumeris.com/wp-content/uploads/2017/06/Payment-refom-chart_4A-2.png
https://pmc.ncbi.nlm.nih.gov › articles
It is a consensus that Fee for Service FFS is a traditional medical insurance payment scheme with significant disadvantages namely the waste of health care resources

https://pmc.ncbi.nlm.nih.gov › articles
Reimbursement mechanisms for healthcare have included salary Fee for service FFS capitation Pay for performance P4P and diagnosis based payment DRGs diagnosis

AddictionCertificationsTrainings

Racial Health Disparities In Michigan Declined According To COVID Task
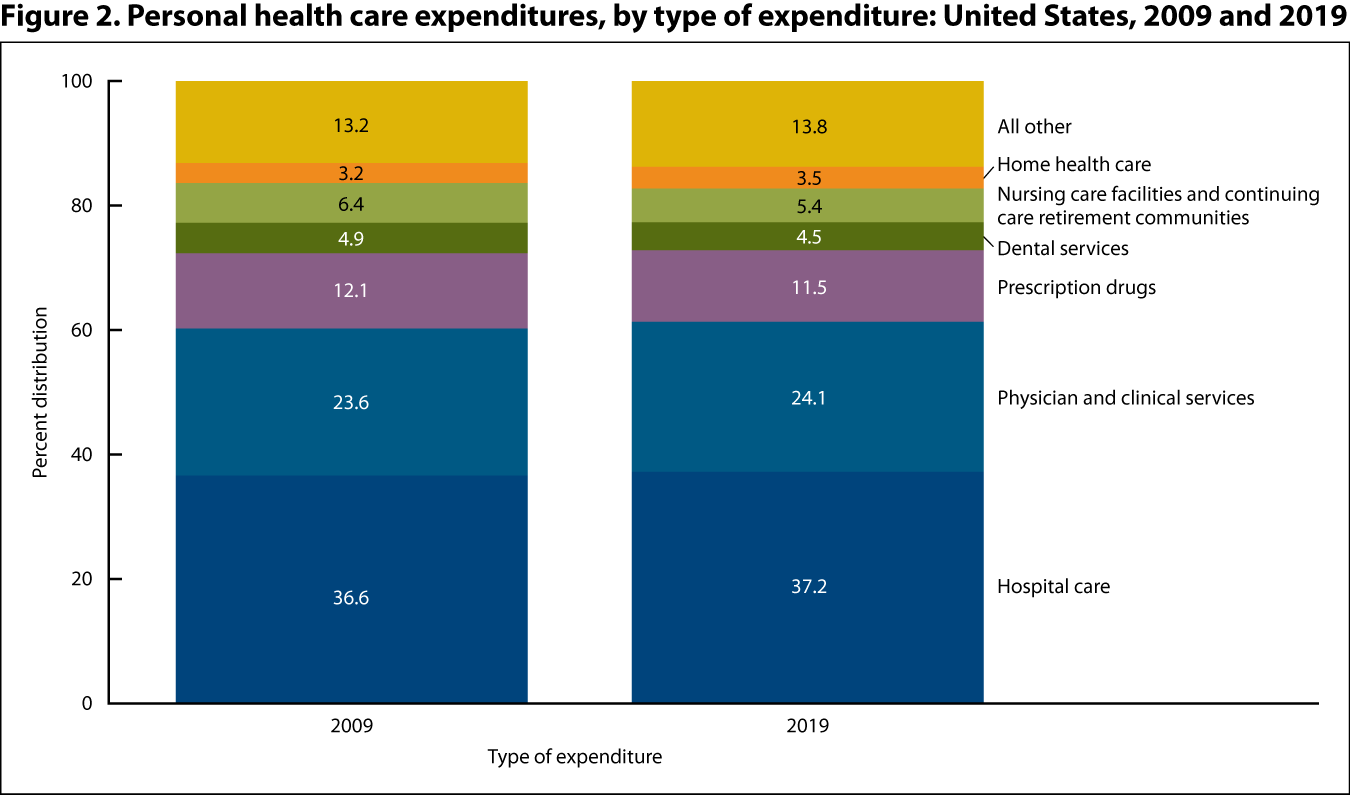
Health Care Expenditures Health United States
Healthcare Reimbursement How It Works For Providers

Mubeen Kamani Anticipated Time Of Iftar

Future Of Improved Livability Robust Accommodation In The NDIS

Future Of Improved Livability Robust Accommodation In The NDIS
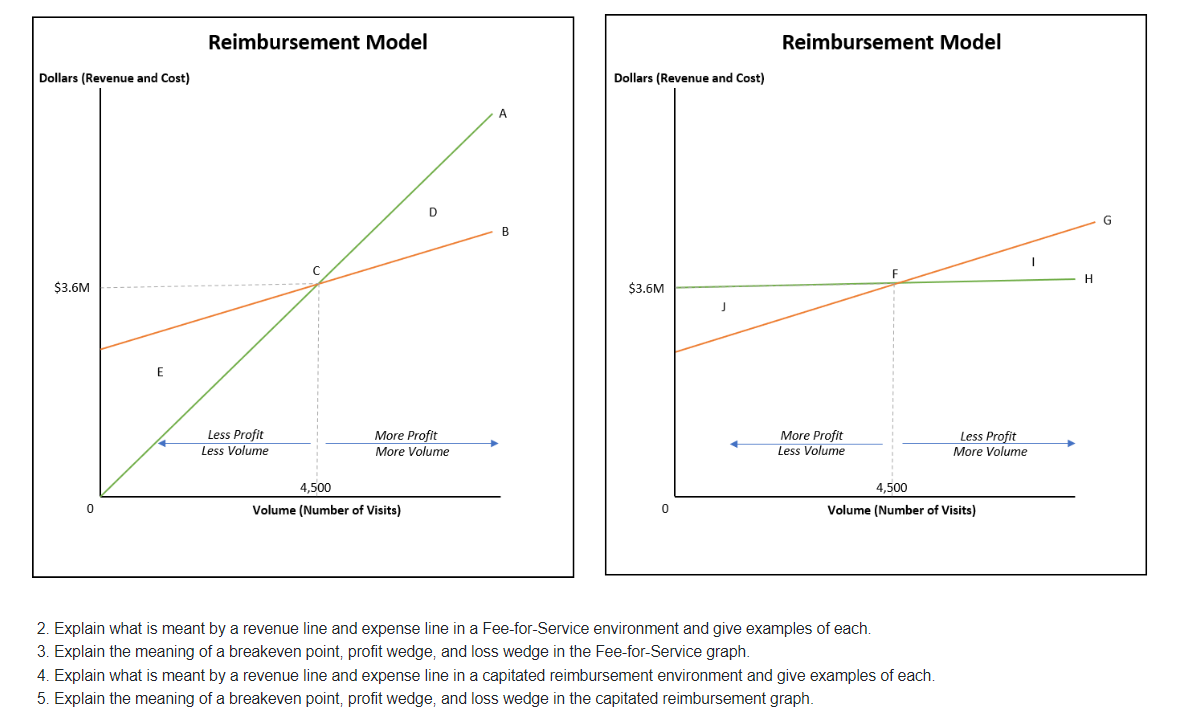
Solved 1 Given Revenue volume Graphs For A Medical Practice Chegg
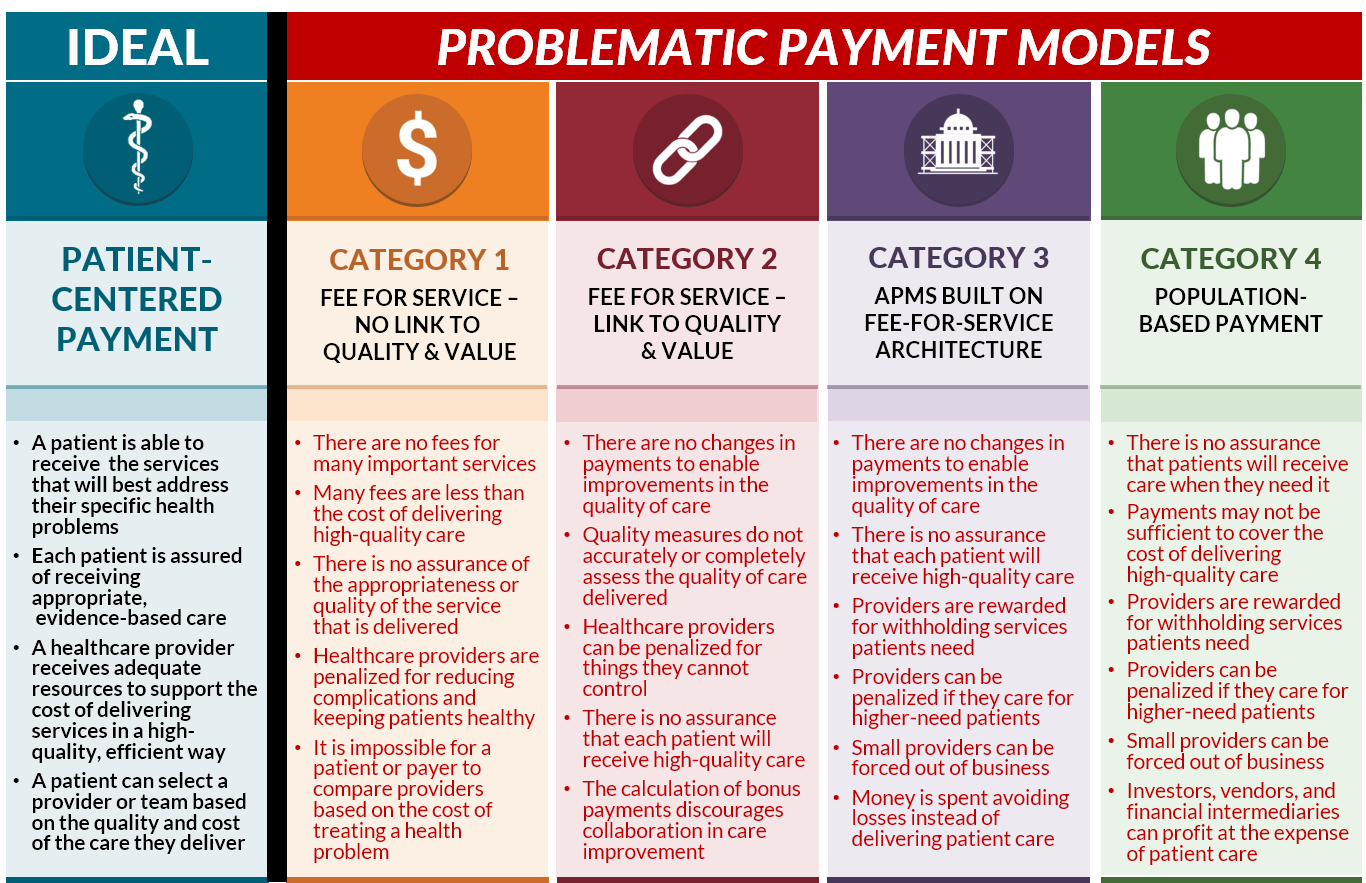
Problems With Current Value Based Payments

What The Aged Care Task Force Means For Retirement Village Operators
Fee For Service Reimbursement Systems Help Reduce Health Care Expenditures - Many healthcare policymakers and researchers argue that fee for service payment mechanisms provide a strong economic incentive to overprovide services many of which are costly